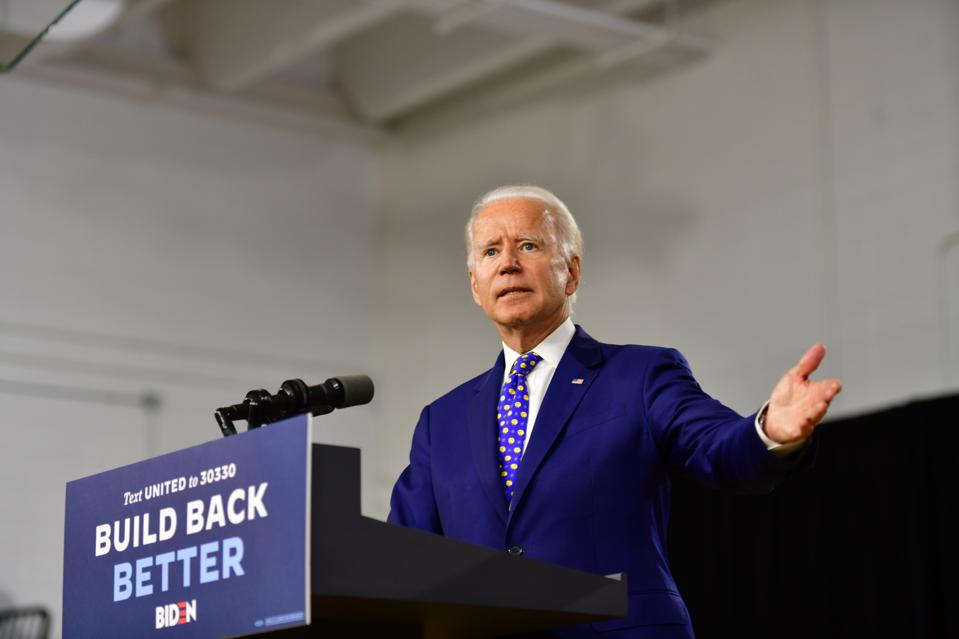
Biden mentions wellness design program for low income seniors in campaign speech about community and … [+]
Getty Images
It’s rare that wellness design, the growing practice of creating built spaces that support the well-being of their occupants, shows up in presidential campaigns, but it made an appearance in a policy speech Democratic nominee Joseph R. Biden Jr. gave in late July and streamed on Facebook Live. Here’s how he tied it into his healthcare policy-focused talk:
“There’s a pilot program now in 27 cities and 16 states where a nurse, an occupational therapist and a handyman come to the home that’s caring for an aging family member. They might not be able to cure Mom’s Alzheimer’s, but they can make sure she doesn’t break her hip. So they walk through the house… and they install handrails in the rights spots in the house and bathroom, or they fix the door that’s stuck so she doesn’t trip when she tries to open it. It initially found that about $3,000 in program costs yielded more than $20,000 in savings to the government, from hospitalizations and other reasons.”
Campaign Cameo Surprises Program Creator
The wellness design program Biden described is called CAPABLE, a descriptive acronym for Community Aging in Place – Advancing Better Living for Elders, developed at Johns Hopkins School of Nursing. It was the brainchild of Sarah L. Szanton, a nursing professor and director of the school’s Center for Innovative Care in Aging.
She did not know it would come up in Biden’s campaign, she says, or that he was aware of it. “It was a fun surprise,” she muses, suspecting that his staff shared it with him recently, rather than him remembering it from his days in the Obama administration when the program began. “People from other campaigns had reached out during the primaries but not Biden,” she recalls.
Affordable Wellness Design Program for Low Income Seniors

Elderly woman holding on handrail for safety walk steps.
getty
What makes it notable? “No other program addresses function from a prevention point of view, by addressing the person and their home environment,” Szanton shares. CAPABLE covers four environmental areas:
- Structural adaptations include widening doors for wheelchair access, adapting showers, installing non-slip flooring and installing grab bars;
- Home repairs include fixing holes and broken lights, securing loose carpet and un-sticking the doors Biden mentioned to eliminate trip and fall hazards;
- Assistive devices include raised toilet and shower seats and reachers to make accessing items easier;
- Regular household items include fire extinguishers, night lights and desk lamps, sturdy nonslip rugs and mats.
These items cost anywhere from $5 to $500, a modest expense for adding safety and functionality to an older resident that can save thousands in healthcare costs related to hospital stays. “Currently, Medicaid pays for it in Massachusetts,” Szanton says. “Other than that, it has been either philanthropy or value-based payment insurers who believe they will achieve the savings we did.” (They have, studies show.)
In cases where the client is a tenant, rather than a homeowner, the property owner has to give permission for the modifications. This hasn’t been a barrier, Szanton observes. “We haven’t had any landlords deny permission.” Some say they will perform the modifications themselves. Others allow the program’s handymen to do them. (Those are selected by the program sites, she notes, with nonprofits like Civic Works participating.)
Health Policy Success Story
In a three-year test starting in 2012, CAPABLE enrolled 281 adults aged 65 and older who were eligible for Medicare and Medicaid, had difficulty performing daily living tasks and experienced related depression at their loss of functionality. Reporting results in the prestigious Journal of the American Medical Association in 2019, Szanton and her colleagues wrote, “Participants in the CAPABLE group vs. those in the control group were more likely to report that the program made their life easier, helped them take care of themselves, and helped them gain confidence in managing daily challenges.” The JAMA study concluded: “Low-income community-dwelling older adults who received the CAPABLE intervention experienced substantial decrease in disability.”
Looking at the program’s impressive results, Szanton says, “In June 2019, the PTAC committee voted to recommend traditional Medicare should scale CAPABLE in a limited way to test continued cost-effectiveness.” PTAC is the Physician-Focused Payment Model Technical Advisory Committee within the Department of Health & Human Services’ planning and evaluation office.
Expansion Possibilities
HHS Secretary Azar has been encouraging, Szanton notes, which could mean possible program expansion regardless of which candidate wins the election. What might that look like in terms of funding? Szanton sees four possibilities: “It could be paid for as a bundle of services by Medicare. It could be part of the Annual Wellness Visit (that already screens for how functional someone is. That visit could be at home and then could be a referral (if needed) to CAPABLE. Medicare Advantage programs could be given blanket approval to offer CAPABLE through their supplemental benefits activities. The [Medicare and Medicaid Dual Eligibility Special Needs Plans] could be encouraged to offer CAPABLE.”
Any of these approaches would be building on a record of success: “So far, all organizations who have tried CAPABLE have saved money and improved participant engagement.” While Biden cited 27 CAPABLE cities in his speech, Szanton reports that it’s now in 30 places, with expansion coming soon. Existing organizations include the National Center for Healthy Housing, Trinity Health system in Michigan, SCAN health system in California and Colorado Visiting Nurse Association.
Best Possible Outcomes

Restoring functionality to seniors’ lives reduces depression and injury risk.
getty
What’s most valuable about CAPABLE isn’t the home improvements or healthcare savings, Szanton believes: “The real strength is addressing people’s own functional goals. Participants achieve them partly through environmental changes, but it is much more about building self-efficacy for what they actually want to do – to go out their front stairs, take a walk, stoop to feed their dog without pain, etc.”
Helping Mom enjoy the later years of her life while avoiding ending up in the hospital with a broken hip is the best possible outcome for her and her family. Lowering Medicare and Medicaid costs is a worthwhile outcome for the federal government, states and taxpayers.
