Hospital design experts Bryan Langlands and Teri Oelrich explains how healthcare facilities can make creative use of their spaces in order to reduce the social isolation felt by healthcare workers and patients.
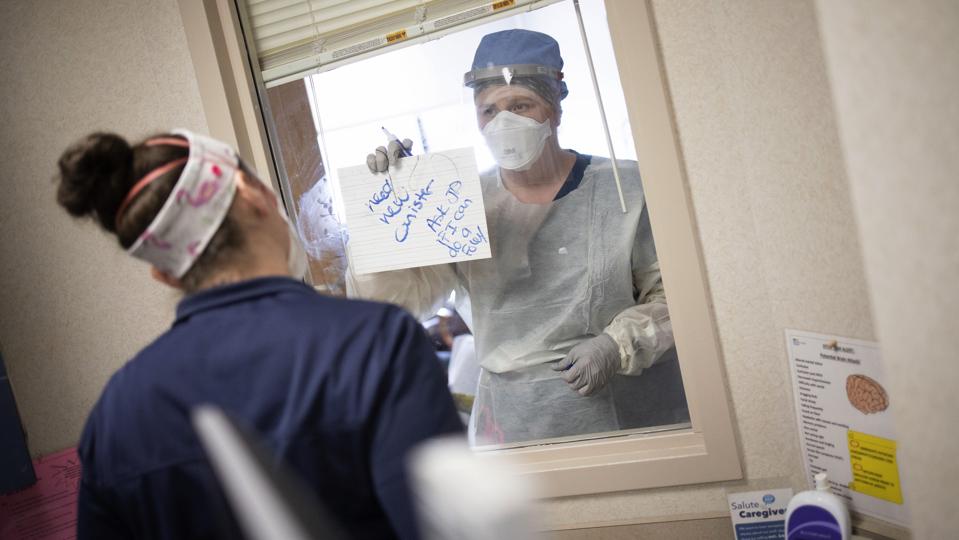
To reduce the number of times a patient’s room door is opened and the amount of personal protective … [+]
Win McNamee/Getty Images
Covid-19 increases social isolation for almost everyone, but especially for caregivers on the frontlines and patients in hospitals. This is in part due to critical infection prevention systems, safety protocols and social distancing measures, such as multiple layers of PPE, single-patient isolation rooms and no-visitor policies.
Studies reveal isolation, which can lead to loneliness, can both increase anxiety and depression as well lower trust, energy and social engagement. Yet despite countless conversations with healthcare workers on the front lines — from nurses to pastoral care — who say social isolation is a challenge for both caregivers and patients, there is hope. Below are key insights from these discussions, as well as strategies to create environments that ease isolation.
How to combat the effects of isolation
Because of the increased isolation due to Covid-19, the pandemic takes a toll on both extroverted and introverted staff. Extroverted staff that gain energy from social interactions may have a more difficult time than introverts, who typically enjoy more time alone. Yet while it may be easier for introverts to cope in the short term, introverts need social time as well in addition to downtime that’s not just with a patient. For example, in conversations with frontline workers, they report missing the after-work informal socialization at restaurants and bars. How can caregivers be connected to others so they’re not fighting the battle by themselves? Here are a few strategies that may help.
Offer space for enhanced communication
Studies show that body language may account for up to 65% of all communication or more, so it’s crucial to employ innovative ways to communicate. Masks and PPE hide dialogue, greetings and facial cues, which are all crucial ways to convey not just critical patient information, but also ideas, feelings and beliefs.
Clinical staff who work with patients on isolation could use glass doors to communicate with colleagues outside the room by writing notes to each other on the transparent surface. In addition, digital and analogue message walls can provide opportunities for staff to share more informal, personal notes of encouragement that can be pushed from their smartphone or posted via sticky notes. Furthermore, nursing units with decentralized nurse stations could help minimize social isolation.
Boost opportunities to personally connect
It’s important for caregivers to share experiences and connect personally outside of work tasks, as well as celebrate milestones and work successes. Staff potlucks, birthdays and holiday celebrations are a mainstay on nursing units, and an important way for staff to interact and connect with one another.
In feedback from frontline caregivers, there are valuable opportunities to provide better break rooms. These areas could feature operable windows for fresh air, sunlight, and views of green plants, to not only create a more pleasant space for socializing, but to help boost mood, improve cognition and decrease stress. The size of break rooms should also be considered if social distancing is required when eating because a room which previously held 10-12 staff might only hold 3-4 now.
Opportunities for caregivers to cultivate mindfulness and seek individual respite allow staff a way to recharge and find ways to cope with the stress of social isolation.
In addition, stairwells and the ends of corridors could serve as places to catch up with colleagues, and instead of places solely dedicated to circulation, they could also serve as destinations. Feedback from staff who work in hospitals where staircases are along glass perimeters of a building tell us that they become a “found” place for restorative respite, to take a moment to pause or to encourage exercise. Staircases with daylight and generous width and landings are highly popular with staff as a place to take phone calls, meet with a colleague, take a “time out” moment, and for some, to even have lunch.
Expansive windows with views, soft bench seating and even small side tables could help create a welcoming environment. These areas could also serve as informal touch down spaces for virtual team building events, such as Zoom coffee breaks, to provide ways for distributed teams to connect. And when able to step away from the floor for a rare longer break, or before or after a shift, easily accessible green roofs and healing gardens are especially important.
Another change since the pandemic has been that hospitals are decreasing the number of entrances and exits to facilities. Staff are usually diverted to one entrance where they can get their scrubs for the day and change their shoes. This area could also be an opportunity to create positive communication and gathering outside this door.
Enable peer support and mindfulness
A solid support system is crucial — especially at work. Employees who have a best friend at work are seven times as likely to be engaged in their job. When people have more friends in the workplace, they are more productive and less stressed. Calming spaces filled with comfortable furniture and soothing lights for healthcare workers to listen to one another and provide emotional support — such as affect labeling or putting feelings into words — as well as planning and problem solving, could help. These rooms could also provide spaces for staff to connect with a virtual therapist.
In addition, opportunities for caregivers to cultivate mindfulness and seek individual respite allow staff a way to recharge and find ways to cope with the stress of social isolation. Multi-sensory decompression rooms filled with gentle lights, sounds of nature and images of a verdant forest, could promote rejuvenating, meditative retreats.

Chuck Choi/NBBJ
Strategies to Decrease Patient Isolation
As many hospitals reduce visitors, social isolation can be incredibly debilitating for patients too. While some hospitals allow one visitor, others maintain a no-visitor policy. Although a hospital with fewer visitors can be a quieter, more restful place, it can be lonely for patients, especially during their most vulnerable times. This is especially true because patients feel more comfortable and trusting of care when a family member is present, not to mention that it helps staff communicate with the family about the patient’s history and medications.
At times, these restrictions also require healthcare workers to take on the role of caregiver, family and friend to their patients. These challenges are also compounded with PPE requirements. In the era of the coronavirus crisis, communication between caregivers and patients is more nuanced and complex. Below are a few ideas to overcome isolation for patients.
Employ creative communication methods
In discussions with caregivers, patients and healthcare staff alike are retraining their communication methods. Many facial expressions and of course speech, are tied to the mouth, but facial coverings mask these cues and soften spoken words. Instead, eye and eyebrow movements may be even more essential to convey meaning. One patient shared that they were not concerned about seeing their caregiver’s face because they “believe that people smile with their eyes.” This patient’s advice was to “focus on what you can see, not what you can’t.”
Increased focus on intentional or physical communication is key: staff can put photos of themselves on their PPE so patients can see what they look like behind their masks, while patients can also include photos of themselves and their families in their rooms. Celebratory rituals could also minimize patients’ isolation. When patients reach a certain milestone, or are discharged from the hospital, upbeat music and simple encouragement can be immensely uplifting.
Offer engaging technology
Technology can bring people closer together and provide positive distractions to help improve the patient experience. Wall-mounted screens in inpatient rooms that work in tandem with patient smartphones and iPads could display medical information and history, but also provide video conferencing,entertainment options and relaxing music. These custom, built-in screens could also provide translation assistance to supplement current services. The post-traumatic stress for staff who have had to hold a phone up to a family member’s ear during their loved one’s last moments or being the vehicle for the patient to Facetime with family who are restricted from visiting is tremendous. We can do better.

Clear signage is a key way to help patients.
Sean Airhart/NBBJ
Streamline entrances and exits
For hospitals that do allow visitors, streamlining entrances and exits with clear, direct signage is critical. For example, using recognizable shapes like circles and unusual colors like pink within the visual signage allows for visitors to navigate their way to, around and through the hospital.
Provide meaningful spiritual care
Spiritual care may offer a powerful means for patients to share their wishes, desires and fears. Within a hospital we tend to focus on the physical and medical, but not the spiritual. Patients who have no visitors want someone to listen to how their lives and their family’s lives have been impacted by their illness. Focusing on spiritual care is essential and can allow patients to reflect on life’s joyous and challenging moments.
A disconnect between caregivers and their work environment, and patients and their families, can create emotional exhaustion. Thoughtful and considered design does not need to come with a high price tag. Look for opportunities in planning and design where a small move can be the difference between functional and generous. From extra inches in stair widths and landings to ending corridors in glass instead of drywall to larger and more staff lounges, these design choices show the emotional well-being of the staff and patient is as important as clinical care and patient safety.
